Note: This article was originally posted on February 16, 2021, and was updated on November 10, 2025.
Introduction
 More than a hundred years ago, Dr. Russell M. Wilder and two Dietitians from the Mayo Clinic wrote a 69-page book titled A Primer for Diabetic Patients – A Brief Outline of the Principles of Diabetic Treatment, Sample Menus and Food Tables [1]. It described how diabetes was managed before the discovery of insulin, using several levels of low-carbohydrate and very low-carbohydrate (ketogenic) diets and short fasting periods. The approach is very similar to current low-carbohydrate and very low-carbohydrate (keto) diets used by those who want to improve or achieve remission of the symptoms of type 2 diabetes using a diet-first approach.
More than a hundred years ago, Dr. Russell M. Wilder and two Dietitians from the Mayo Clinic wrote a 69-page book titled A Primer for Diabetic Patients – A Brief Outline of the Principles of Diabetic Treatment, Sample Menus and Food Tables [1]. It described how diabetes was managed before the discovery of insulin, using several levels of low-carbohydrate and very low-carbohydrate (ketogenic) diets and short fasting periods. The approach is very similar to current low-carbohydrate and very low-carbohydrate (keto) diets used by those who want to improve or achieve remission of the symptoms of type 2 diabetes using a diet-first approach.
Wilder’s Early Work and the Ketogenic Diet
“The effect of ketonemia on the course of epilepsy”
The name Dr. Russell Wilder is best known for his 1921 paper “The effect of ketonemia on the course of epilepsy” [2]. In it, Wilder proposed a very high-fat, low-carbohydrate diet to mimic the benefits of fasting for people with epilepsy. Wilder is the one who coined the term ketogenic diet, and his classic 4:1 ketogenic diet is still used today to manage epilepsy and as an adjunct in treatment for glioblastoma.
While Wilder’s name is tied to epilepsy treatment, his prior work used low-carbohydrate and ketogenic diets in the treatment of diabetes. The answer to why this history was lost lies in timing: just a year after Wilder began this work, Dr. Frederick Banting and Charles Best discovered insulin [3].
Insulin was life-saving for those with type 1 diabetes. However, it is harder to understand why Wilder’s dietary approach did not continue for those with type 2 diabetes, where the body still makes insulin but cannot use it properly. It is possible that because the two types were not clearly differentiated until 1936, insulin became the standard therapy for all “diabetes.”
Determining Carbohydrate Tolerance
Wilder’s approach was to view diabetes as carbohydrate intolerance. He defined carbohydrate tolerance as “the amount of sugar-forming foods which a person can eat in twenty-four hours without causing sugar in the urine.”
 “The actual procedure will vary with different patients, but, in general, foods of known composition in weighted amounts are fed, the total intake of carbohydrate, protein, and fat being increased very gradually as high as possible without the return of sugar in the urine.”
“The actual procedure will vary with different patients, but, in general, foods of known composition in weighted amounts are fed, the total intake of carbohydrate, protein, and fat being increased very gradually as high as possible without the return of sugar in the urine.”
Every patient was treated as an individual case, but for convenience, Wilder made these arbitrary groupings based on tolerance:
- Group A: Below 40 g of carbohydrate.
- Group B: Between 40–60 g of carbohydrate.
- Group C: Between 60–100 g of carbohydrate.
- Group D: Above 100 g of carbohydrate.
Different Daily Macros
Different macros were prescribed based on tolerance. For example, Group A was instructed to eat 20 grams of carbohydrate, 70 grams of protein, and 100 grams of fat at each of 3 meals [1]. These diets provided adequate protein for satiety. Fat came mainly from butter, cream, cheese, and animal protein, while carbohydrates were restricted to low-carb vegetables and small amounts of fruit.
Use of Fasting and Protein-Sparing Fasts
Wilder utilized short fasts of 12–24 hours to improve blood sugar control. Group A was advised a weekly “fast day” with liquids like broth or tea. If sugar persisted in the urine, Wilder prescribed a protein-sparing modified fast:
“If sugar persists, the patient should return to one-half of his diet, continue on this for a week, and then again try the effect of a fast day. After the urine is again sugar-free, he can return gradually to his previous diet.”
From Insulin to Oral Medications
Oral diabetes medications, such as sulfonylureas and Metformin, only became available in the mid-1950s [6,7]. Before this, insulin was the primary treatment for all diabetes. A 1958 paper by Wilder [5] explains how the discovery of insulin led to the decline of low-carbohydrate diets. As insulin became less expensive and widely available, diets focused on carbohydrate restriction were abandoned.
What Was Lost
Perhaps the reason that diabetes has been considered a chronic and progressive disease is that dietary treatment was forgotten. Wilder’s recommendation was simple: “Suit the diet to the condition of the patient and feed no more sugar-forming foods than the patient’s body is able to use [1].”
Today, people with type 2 diabetes can still follow a carbohydrate-reduced diet to manage their blood sugar and potentially discontinue medications. Given these diets are safe and effective, they should be considered a viable diet-first approach.
Revisiting Dietary Treatment
The safety and efficacy of low-carbohydrate and ketogenic diets for diabetes are acknowledged by the American Diabetes Association [8], Diabetes Canada [9], and Diabetes Australia [10].
Crucially, individuals taking insulin must have their doctor de-prescribe medications before adopting a low-carbohydrate diet to avoid hypoglycemia. A 2019 guide in the British Journal of General Practice explains how Physicians can safely manage this medication adjustment [11].
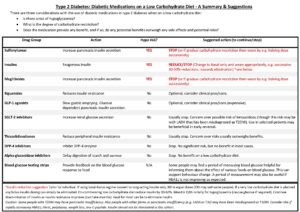
Campbell M. et al, Adapting diabetes medication for low-carbohydrate management [11]
Final Thoughts
Type 2 diabetes remains a disease of carbohydrate intolerance. Every person’s carbohydrate tolerance is different, which is why a personalized low-carbohydrate diet is essential. This is the diet-first approach I offer to help people put the symptoms of type 2 diabetes into remission.
More Info
If you have been diagnosed with type 2 diabetes and would like to take a low-carb or “keto” approach, I would be glad to help. You can view my Comprehensive Dietary Package here and learn about me here.
To your good health!
Joy
You can follow me on:
Twitter: https://twitter.com/jyerdile
Facebook: https://www.facebook.com/BetterByDesignNutrition/
Note: Special thanks to Jan Vyjidak of Neslazeno.cz for locating Wilder’s book, A Primer for Diabetic Patients [1].
References
- Wilder RM, Foley MA, Ellithorpe D. A Primer for Diabetic Patients. Mayo Clinic, W.B. Saunders Co, 1922. [https://archive.org/details/primerfordiabeti00wild]
- Wheless JW. History of the ketogenic diet. Epilepsia. 2008 Nov;49 Suppl 8:3-5. [https://pubmed.ncbi.nlm.nih.gov/19049574/]
- Diabetes.co.uk. The History of Insulin. 2019. [https://www.diabetes.co.uk/insulin/history-of-insulin.html]
- Krochmal M. 10 Facts About the History of Diabetes. Type2Diabetes.com. 2018. [https://type2diabetes.com/living/10-facts-history-diabetes/]
- Wilder RM. Recollections and Reflections on Education, Diabetes, Other Metabolic Diseases, and Nutrition in the Mayo Clinic and Associated Hospitals, 1919–50. Perspectives in Biology and Medicine. 1958;1(3):237-277. [https://doi.org/10.1353/pbm.1958.0024]
- Scheen AJ. History of sulfonylureas. Diabetes Metab. 2004 Oct;30(5):487–492. [https://pubmed.ncbi.nlm.nih.gov/15671911/]
- Bailey CJ, Day C. Metformin: its history and future. Diabetologia. 2019 Mar;62(3):482–487. [https://doi.org/10.1007/s00125-018-4808-3]
- American Diabetes Association. 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020 Jan;43(Suppl 1):S48-S65. [https://pubmed.ncbi.nlm.nih.gov/31862748/]
- Diabetes Canada. Diabetes Canada Position Statement on Low Carbohydrate Diets for Adults with Diabetes: A Rapid Review. Canadian Journal of Diabetes. 2020 Jun;44(4):295-299. [https://doi.org/10.1016/j.jcjd.2020.04.001]
- Diabetes Australia. Position Statement: Low-Carb Eating for People with Diabetes. 2021. [https://www.diabetesaustralia.com.au/wp-content/uploads/Diabetes-Australia-Position-Statement-Low-Carb-Eating.pdf]
- Campbell M, Unwin D, Cavan D, et al. Adapting diabetes medication for low-carbohydrate management of type 2 diabetes: a practical guide. British Journal of General Practice. 2019 Jul;69(684):360-361. [https://pubmed.ncbi.nlm.nih.gov/31249097/]

© 2025 BetterByDesign Nutrition Ltd.

Joy is a Registered Dietitian Nutritionist and owner of BetterByDesign Nutrition Ltd. She has a postgraduate degree in Human Nutrition, is a published mental health nutrition researcher, and has been supporting clients’ needs since 2008. Joy is licensed in BC, Alberta, and Ontario, and her areas of expertise range from routine health, chronic disease management, and digestive health to therapeutic diets. Joy is passionate about helping people feel better and believes that Nutrition is BetterByDesign©.

