Introduction
For as long as I can remember, type 2 diabetes has been called a chronic, progressive disease and people diagnosed with type 2 diabetes have been taught that (1) the disease will persist (i.e. is chronic), (2) will only get worse (i.e. is progressive), (3) that medication to manage the disease is inevitable, and (4) that as the disease progresses multiple medications may be required, including insulin.
A newly published consensus report (August 31, 2021) from an expert panel made up of representatives from the American Diabetes Association (ADA), European Association for the Study of Diabetes (EASD) and Diabetes UK states that “diabetes may not always be active and progressive” [1,2,3], and the report highlights that remission is possible, and a person may need ongoing support and regular monitoring to prevent relapse.
Conventional Perspectives on Disease Progression
The website of the American Diabetes Association states [4];
“You might start managing your diabetes with diet and exercise alone, but, over time, will have to progress to medication, and further down the line you might need to take a combination of medications, including insulin.”
While this will be the case if diet and lifestyle are not adequately changed, but it is by no means inevitable!
Diabetes Canada, in its patient resources on “the basics” of type 2 diabetes, states,” type 2 diabetes is a progressive, life-long disease” [5]
…and in its March 2020 handout on access to diabetes medication states, Diabetes Canada states that: [6];
Diabetes is a chronic, progressive disease that affects the body’s ability to regulate the amount of glucose (sugar) in the blood. It has no cure, but can be managed through education, support, healthy behaviour interventions, and medications.
…and in its advocacy report on bariatric surgery as a type 2 diabetes intervention strategy [7] states;
Diabetes is a chronic, progressive disease affecting more than 3.6 million Canadians; approximately 90 per cent of whom live with type 2 diabetes. Type 2 diabetes is caused by a combination of genetic, lifestyle and environmental factors. It occurs when the body cannot properly regulate the amount of glucose (sugar) in the blood. Insufficient insulin production, insulin resistance, or both, cause hyperglycemia (high blood sugar) which, over time, can damage blood vessels, nerves and organs, and lead to many debilitating and irreversible complications. Type 2 diabetes can be managed with education and support, behaviour interventions (including healthy eating, regular physical activity and stress reduction) and medication.
Evidence-Based Pathways to Type 2 Diabetes Remission
Why do diabetes associations not explain that there are three documented ways to put type 2 diabetes into remission, two of which are dietary?
- A ketogenic diet [8,9]
- A low-calorie energy-deficient diet (calorie restriction) [10,11,12]
- Bariatric surgery (especially use of the Roux-en-Y procedure) [13,14]
Why are people diagnosed with type 2 diabetes still told that type 2 diabetes is a chronic, progressive disease — rather than told about the two evidence-based dietary options to achieve remission?
Final Thoughts…
In light of this new consensus report stating that “diabetes may not always be active and progressive” [1,2,3], it is time to stop referring to diabetes as “a chronic, progressive disease”.
People need to know that remission is possible, as well as information about the evidence-based dietary options that can lead to remission.
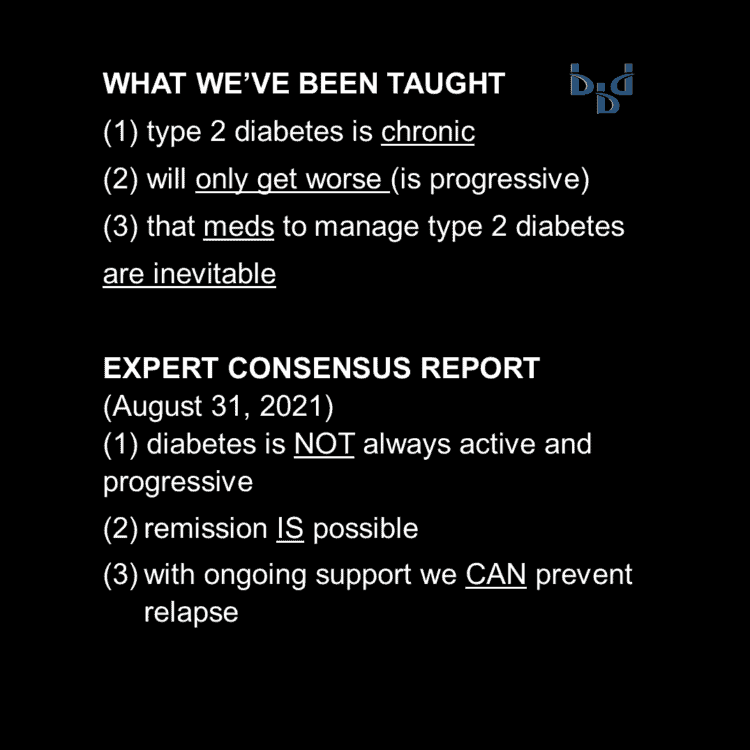
What We’ve Been Taught and What We Need to Know
More Info
Learn about me and how I can support you in pursuing remission of type 2 diabetes. You can view my Comprehensive Dietary Package here.
To your good health!
Joy
You can follow me on:
Twitter: https://twitter.com/jyerdile
Facebook: https://www.facebook.com/BetterByDesignNutrition/
References
- Riddle MC, Cefalu WT, Evans PH, et al. Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. J Clin Endocrinol Metab. 2021;106(11):3333-3341. doi:10.1210/clinem/dgab585 [https://academic.oup.com/jcem/article/106/11/3333/6358409]
- Riddle MC, Cefalu WT, Evans PH, et al. Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. Diabetes Care. 2021;44(10):2438-2444. doi:10.2337/dci21-0034 [https://diabetesjournals.org/care/article/44/10/2438/138556/Consensus-Report-Definition-and-Interpretation-of]
- Riddle MC, Cefalu WT, Evans PH, et al. Consensus report: definition and interpretation of remission in type 2 diabetes. Diabetologia. 2021;64(11):2359-2366. doi:10.1007/s00125-021-05542-z [https://link.springer.com/article/10.1007/s00125-021-05542-z]
- American Diabetes Association. How Type 2 Diabetes Progresses. 2021. [https://www.diabetes.org/diabetes/how-type-2-diabetes-progresses]
- Diabetes Canada. Type 2 diabetes – the basics. Patient Resource. 2021. [https://guidelines.diabetes.ca/docs/patient-resources/type-2-diabetes-the-basics.pdf]
- Diabetes Canada. Access to Diabetes Medication, March 2020. Advocacy Report. [https://www.diabetes.ca/DiabetesCanadaWebsite/media/Advocacy-and-Policy/Advocacy%20Reports/Access-to-Diabetes-Meds_Time-to-Listing_EN.pdf]
- Diabetes Canada. Bariatric surgery as a type 2 diabetes intervention strategy. Advocacy Report. 2021. [https://www.diabetes.ca/advocacy—policies/advocacy-reports/bariatric-surgery-as-a-type-2-diabetes-intervention-strategy]
- Hallberg SJ, McKenzie AL, Williams PT, et al. Effectiveness and Safety of a Novel Care Model for the Management of Type 2 Diabetes at 1 Year: An Open-Label, Non-Randomized, Controlled Study. Diabetes Ther. 2018;9(2):583-612. doi:10.1007/s13300-018-0373-9 [https://pubmed.ncbi.nlm.nih.gov/29417495/]
- Athinarayanan SJ, Adams RN, Hallberg SJ, et al. Long-Term Effects of a Novel Continuous Remote Care Intervention Including Nutritional Ketosis for the Management of Type 2 Diabetes: A 2-Year Non-randomized Clinical Trial. Front Endocrinol (Lausanne). 2019;10:348. doi:10.3389/fendo.2019.00348 [https://pubmed.ncbi.nlm.nih.gov/31231311/]
- Lim EL, Hollingsworth KG, Aribisala BS, et al. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. 2011;54(10):2506-2514. doi:10.1007/s00125-011-2204-7 [https://pubmed.ncbi.nlm.nih.gov/21656330/]
- Steven S, Hollingsworth KG, Al-Mrabeh A, et al. Very Low-Calorie Diet and 6 Months of Weight Stability in Type 2 Diabetes: Pathophysiological Changes in Responders and Nonresponders. Diabetes Care. 2016;39(5):808-815. doi:10.2337/dc15-1942 [https://pubmed.ncbi.nlm.nih.gov/27002059/]
- Lean MEJ, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. 2018;391(10120):541-551. doi:10.1016/S0140-6736(17)33102-1 [https://pubmed.ncbi.nlm.nih.gov/29221645/]
- Cummings DE, Rubino F. Metabolic surgery for the treatment of type 2 diabetes in obese individuals. Diabetologia. 2018;61(2):257-264. doi:10.1007/s00125-017-4513-9 [https://pubmed.ncbi.nlm.nih.gov/29204739/]
- Madsen LR, Baggesen LM, Richelsen B, et al. Effect of Roux-en-Y gastric bypass surgery on diabetes remission and complications in individuals with type 2 diabetes: a Danish population-based matched cohort study. Diabetologia. 2019;62(4):611-620. doi:10.1007/s00125-019-4816-2 [https://pubmed.ncbi.nlm.nih.gov/30728989/]

© 2025 BetterByDesign Nutrition Ltd.

Joy is a Registered Dietitian Nutritionist and owner of BetterByDesign Nutrition Ltd. She has a postgraduate degree in Human Nutrition, is a published mental health nutrition researcher, and has been supporting clients’ needs since 2008. Joy is licensed in BC, Alberta, and Ontario, and her areas of expertise range from routine health, chronic disease management, and digestive health to therapeutic diets. Joy is passionate about helping people feel better and believes that Nutrition is BetterByDesign©.
