Approximately 90% of Canadians (87%) have extended health benefit plans; 64% of people have them through their employer, another 14 % access them through another type of group plan, and 9% of people buy private health insurance [1] and most major insurers (7 out of 10) cover Registered Dietitian services in their standard plan [2].
While all Canadian insurers provide coverage for Registered Dietitian services [3], each individual company chooses to purchase (or not) different amounts of coverage for their employees. As a result, insurance coverage varies significantly company to company, even with the same insurer, so it’s important to check with your insurer, or group benefits representative to determine what your yearly limits are for coverage for a Registered Dietitian, as well as how much they cover per visit.
Yearly Limits
Yearly limits for Registered Dietitian services on extended benefits plans frequently range from $500/year to $1500/year however this is only one aspect of what determines the amount that each insurer will reimburse.
Reasonable and Customary Fees
In addition to yearly limits, each plan sets how much they will cover per visit.
Some benefit plans set out how much they will cover for the initial assessment visit and how much they will cover for each subsequent visit. Other plans reimburse the same amount per visit, regardless if it is the initial assessment visit or not — up to the maximum of the yearly limit.
The insurer uses what is called “reasonable and customary fees” to determine the basis for pricing their benefit plans, as well as the basis for reimbursing claims, and these limits are based on the usual cost for a service in each province.
Multi-Province Dietetic Registration
Since the “reasonable and customary fee” is based on the usual cost for the service in each province, my clients in British Columbia, Alberta and Ontario (the three provinces that I am licensed in) have different reasonable and customary amounts related to my services.
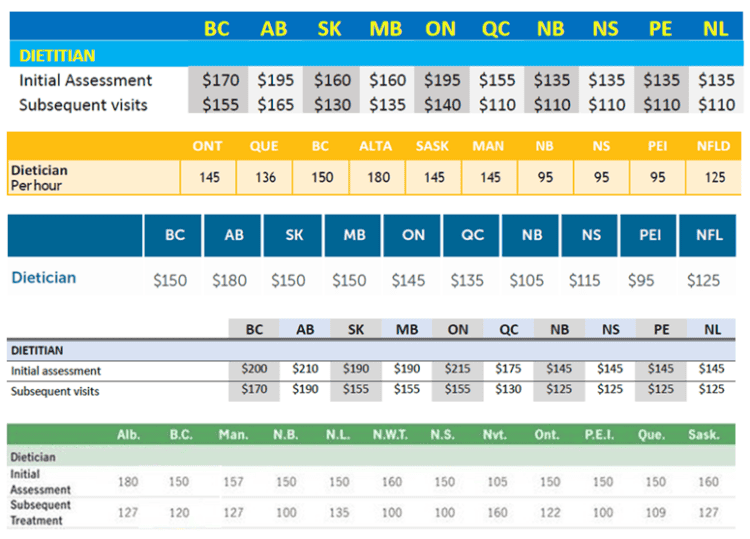
Below are the reasonable and customary limits for Dietitian services from five of the major benefit insurers in Canada. As can be seen, the range that the same provider covers in each province for the same service varies widely.
In pricing my services, I not only take yearly limits into consideration, I also factor in the reasonable and customary fee amounts in each province that I am licensed.
British Columbia – reasonable and customary limits
For an initial Assessment visit to a Registered Dietitian, benefit plans in British Columbia reimburse from $200/hour, to $180/hour, to $170/hour, to $150/ hour.
For subsequent visits to a Registered Dietitian, benefit plans in British Columbia will reimburse from $170/hour, to $155/hour, to $150/ hour, to $120/hour.
Alberta – reasonable and customary limits
For an initial assessment visit to a Registered Dietitian, benefit plans in Alberta will reimburse from $210/hour, to $195/hour, to $180/hour.
For subsequent visits to a Registered Dietitian, benefit plans in Alberta will reimburse from $190/hour, to $180/hour, to $165/hour, to $150/ hour, to $127/hour.
Ontario – reasonable and customary limits
For an initial assessment visit to a Registered Dietitian, benefit plans in Ontario will reimburse from $215/hour, to $195/hour, to $150/ hour, to $145/hour.
For subsequent visits to a Registered Dietitian, benefit plans in Ontario will reimburse for from $155/hour, to $145/hour, to $140/ hour, to $122/hour.
Pricing Based on Inter-Provincial Reasonable and Customary Fee Limits
When planning to go to any paramedical practitioner, including Registered Dietitians, it is important that people keep in mind that because of these reasonable and customary fee limits, how receipts are issued determines how much reimbursement they will get. Packages must broken down into the individual services that make up the package, and each service must have the date and time it was provided, and the individual cost for that service.
I ensure that the receipts provided contain all the information that a client’s benefits plan requires, so that reimbursement is maximized, and occurs quickly. Since many extended benefits plans reimburse per visit, all the packages that I offer are broken down into their respective services, beginning with the Initial Assessment visit, and each subsequent visit. The date and time of each service is listed, and the cost of each
As of January 1, 2026, prices for both an assessment visit and subsequent visit remain at the lower end of the Reasonable and Customary Fee Limits for all three provinces in which I am licensed.
Final Thoughts…
The amount that each extended benefits plan reimburses for visits to a Registered Dietitian is based on the reasonable and customary fees in each province.
If you would like to learn about the many Routine Services, Digestive Health Services, and Therapeutic Diet Services that I provide please have a look the Services tab and to learn about pricing, payment options, and clinical hours, please visit the Book an Appointment tab.
Please check your with your plan provider or company benefits representative to find out what your specific extended benefit plan covers.
To your good health,
Joy
You can follow me on:
Twitter: https://twitter.com/jyerdile
Facebook: https://www.facebook.com/BetterByDesignNutrition/
References
- Coletto, David, Abacus Data, “Canadians and Health Care: Workplace and Group Insurance Plans”, April 6, 2023, https://abacusdata.ca/healthcare-canadians-clhia-workplace-and-group-insurance-plans/
- Dietitians of Canada, “Dietitians are the Best Choice for Employee Benefit Plans”, https://www.dietitians.ca/Advocacy/Priority-Issues-(1)/Dietitian-coverage-on-employee-benefits-plans
- Dietitians of Canada, “Providing access to nutrition services in employee health benefits plans”, https://www.dietitians.ca/Advocacy/Priority-Issues-(1)/Dietitian-coverage-on-employee-benefits-plans/Nutrition-Services-(Test)
Copyright ©2024 BetterByDesign Nutrition Ltd.
LEGAL NOTICE: The contents of this blog, including text, images and cited statistics as well as all other material contained here (the ”content”) are for information purposes only. The content is not intended to be a substitute for professional advice, medical diagnosis and/or treatment and is not suitable for self-administration without the knowledge of your physician and regular monitoring by your physician. Do not disregard medical advice and always consult your physician with any questions you may have regarding a medical condition or before implementing anything you have read or heard in our content.